WANT THE CONFIDENCE THAT COMES WITH
KNOWING YOU LOOK YOUR BEST?
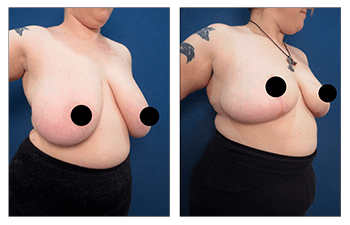
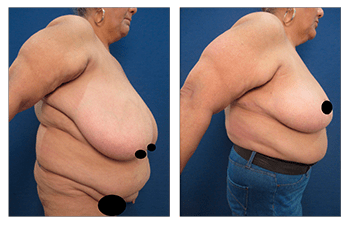
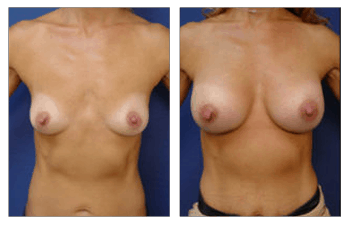
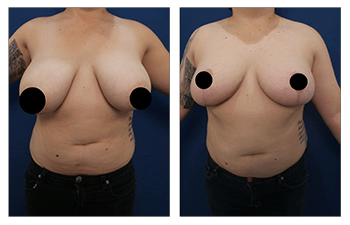
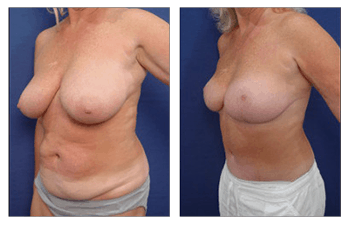
Breast Reduction CASE STUDIES
breast reduction case studies
Breast Reduction
Orange County Breast Reduction is ideal for patients who have observed increase breast volume in addition to sagging of the breast mound and nipple areola complex. Patients may notice enlargement of their breasts at an early age, even as young as their teenage years, termed juvenile breast hypertrophy, or may have observed gradually increase in breast size especially following weight gain and/or pregnancy.
Breast Reduction patients seek results that are opposite of those who undergo a breast augmentation procedure; breast reduction patients want to reduce their breast size.
Patients whose enlarged breasts have become a burden to their routine daily living are characterized as having symptomatic breast hypertrophy. Patients who present with symptomatic breast hypertrophy may qualify for coverage of their bilateral breast reduction surgery through their medical insurance company. Patients with symptomatic breast hypertrophy will routinely complain of upper back and neck strain that prevents them from daily activities such as exercise or of rashes in the inframammary crease that cause them intermittent pain requiring frequent anti-fungal topical cream therapy.
For medical insurance to cover this procedure, patients must demonstrate a lack of bony pathology in the spine as well as the inability to improve upper back and neck pain symptoms despite a six-month trial of anti-inflammatory medications. These concerns can be documented during your breast reduction consultation with Dr. Paris.
Procedure
Enhanced shape, proportionality, and physical comfort of breasts by
- removal of excess glandular tissue, fat, and skin from large breasts,
- lifting and shaping the new contour of the breast,
- adjustment of nipple and areola shape and position, and
- possible liposuction of excess fat from the armpit area.
Length
2 to 4 hours of operative time depending on the amount of reduction.
Anesthesia
General anesthesia.
Place of Treatment
Outpatient surgical suite or hospital operating room.
Side Effects
a) Numbness: Swelling after surgery usually results in loss of feeling in the breast and nipple area during the first several weeks. This impairment should be temporary and last no longer than a few months. In some cases, the loss of feeling can last longer or become permanent due to possible nerve damage or reduced blood supply to the breast.
b) Scarring: Incisions may be lumpy and red for a few months, but they become less apparent over time and can even fade to thin white lines. Healing scars can usually be covered completely by your bra or swimsuit. Please note that smoking impedes the healing process and typically results in more prominent surgical scars.
c) Breast/Nipple asymmetry: Breasts may not be the same size and shape and nipples could be positioned unevenly depending on the degree of preoperative asymmetry.
d) Nursing problems: Women may not be able to breast-feed since the surgery removes many of the milk ducts leading to the nipples.
Risks
a) Hematoma: Hematoma refers to the accumulation of blood in the early postoperative period which pools into a pocket. Hematomas provide a perfect medium for harboring the growth of bacteria. So if you have an infection anywhere in your body, the bacteria will travel through the bloodstream and grow in the hematoma; this can lead to an infection as well as an open wound. In order to avoid a hematoma, drains can be placed in surgery so that any fluid accumulation can be drained. Drains are usually kept in place for 4 to 5 days. In addition, patients are checked preoperatively to make sure that they do not have a blood clotting deficiency.
b) Seroma: Seroma formation refers to the accumulation of plasma fluid in pockets created by the surgical elevation of the soft tissue and disruption of lymphatic vessels. This fluid accumulates due to a low blood count and protein deficiency, both of which may be present in breast reduction patients. This fluid can be a nuisance to patients requiring several aspirations in the office prior to their resolution. More importantly, these plasma fluid pockets may harbor bacterial growth and result in a clinical infection. Drains can be placed in surgery are very effective in preventing seroma formation.
c) Infection: An infection can occur after breast reduction surgery. The infection will disrupt the incision line and may leave the patient with an open wound. Prolonged antibiotics are required to fight the infection and to prevent further extension of the infection. Infections are usually avoided by using the sterile technique, using intra-operative antibiotics, and sealing all incisions sites so that bacteria can’t get in through external contact. In addition, infections are less likely in patients who don’t smoke cigarettes or in patients who quit smoking for at least 1 month prior to surgery.
d) Pulmonary embolism: Blood clots in large veins (deep vein thrombus) may travel up to the heart and lungs and cause pulmonary embolisms (a blockage of the pulmonary artery or one of its branches). Pulmonary embolisms are the leading cause of death after surgery but do not commonly develop.
Recovery
Patients will have a full recovery within 6 weeks of surgery. Patients will be able to return to work if it is not strenuous within two weeks of surgery. Patients will be allowed to wear a sports bra as early as 2 weeks following surgery and all routine undergarment following 4 weeks of surgery.
Duration of Results
Breast reduction surgery typically yields permanent results. However, changes in breast size and shape can happen due to pregnancy, weight gain, or weight loss requiring minor revision surgery.
FREQUENTLY ASKED QUESTIONS
What is the history of breast reduction surgery?
Breast reduction surgery has been performed on patients for more than 20 years, but was not popularized until about 6 to 8 years ago. The rising popularity of breast reduction surgery is probably related to the growing trend for women to be more active and athletic socially and thus desiring less bulky breasts that might limit physical activity. In addition, identification of symptoms associated with breast reduction such as upper back and neck pain and shoulder grooving have resulted in insurance companies often covering this surgery. As such, modern breast reduction surgery has become among the top 6 reconstructive cosmetic surgery operations.
Am I a good candidate for breast reduction surgery?
You may be a good candidate for breast reduction if you have/experience:
- breasts that are too large in proportion to your body
- breasts that are not the same size
- back, neck, or shoulder pain as a result of your breast size
- pendulous breasts with nipples and areolas pointing downward
- skin irritation under your breasts
- inability to participate in various physical activities as a result of your breast size
- dissatisfaction with your breast size.
Breast reduction surgery is typically recommended for women who have completed their breast development. However, breast reduction can be performed at a younger age in teenagers who experience unusual growth of their breasts, termed juvenile breast hypertrophy.
What does breast reduction surgery involve?
Breast reduction surgery can be performed with a variety of techniques, but the procedure is almost always performed using general anesthesia. Usually, your plastic surgeon makes an incision similar in shape to an anchor or an inverted keyhole from the top of the nipple to the natural fold under the breast called the inframammary crease. Then, excess fat, skin and tissue are removed and the remaining skin and areola are repositioned. During surgery, the nipple and areola are kept connected to their sensory nerves and their nutrient vessels and are moved up on the breast mound to correct nipple areola sagging. Although various techniques have been described and are performed routinely, all techniques result in significant reduction of breast size and in improved breast contour shape and nipple areola projection. Excess skin is trimmed around the nipple areola complex and the remaining breast tissue is tucked around the nipple areola complex. Remaining skin on each side of the breast are moved around the nipple areola complex in order to support their lifted position.
Breast reduction by liposuction only is the newest method of reduction and has advantages such as: preservation of breast and nipple sensation, increased likelihood of breastfeeding ability after surgery, less physical trauma to the breast tissue, and minimal risk of complications and scarring. However, breast reduction by liposuction is suitable for few candidates who have enlarged breasts with excellent skin elasticity and have none sagging nipple areola complexes.
How do I plan my breast reduction surgery?
On your initial visit, your surgeon will evaluate your health status by obtaining blood work. If you are 40 years or older or if you have had a personal or family history of breast symptoms (tenderness, lumps, nipple discharge) you will have to obtain a mammogram. If you are a smoker, you should quit for 1 month prior to your breast reduction surgery to minimize the risks of implant infection. In addition, it is prudent to quit smoking for 6 weeks following surgery to ensure a well-healed surgical incision line. Finally, you will need to arrange for a friend or a spouse to care for any small children who may need to be lifted since you will be sore for the first couple days following surgery.
How do I prepare for breast reduction surgery?
Since your surgery will require general anesthesia you must take several precautions prior to surgery. First, you will have to avoid eating and drinking after midnight on the day before surgery. This precaution ensures that your stomach is clear of digested foods that could potentially be aspirated into your lungs during induction of anesthesia. Since, you will have anesthetic medications administered throughout the case; you will remain groggy for several hours and will require a ride to and from the surgery center. You should choose a caretaker who is conscientious and who can spend the first night with you.
What results can I expect after breast reduction surgery?
Breast reduction surgery can alleviate the symptoms associated with large breasts such as: back and neck pain, shoulder strain, skin irritation, poor posture, difficulty participating in strenuous sports activities, difficulty fitting in clothes, and/or self-consciousness created by dissatisfaction with your breast size. This procedure not only eliminates physical discomfort and limitations, but it can also improve the appearance of your breasts. As long as patients do not have significant weight gain or loss and do not become pregnant, they can enjoy a lifetime of comfortable and aesthetically pleasing breasts.
Women who have gained or lost a significant amount of weight may consider breast reduction surgery to make their breasts more proportional to their new body frame and to correct a drooping breasts. Women naturally born with asymmetrical breasts, or those who have asymmetrical breasts following mastectomy on one side can also benefit from breast reduction surgery. Men are also likely to undergo breast reduction surgery to correct the size of enlarged breasts. Regardless of the motivation for surgery, a thorough preoperative assessment, safe intraoperative course, and close monitoring with frequent postoperative visits ensures that patients experience a speedy recovery and a return to a more productive and rewarding life. Patients are usually extremely pleased with breast reduction surgery and radiate increased physical and mental confidence.
Where will my breast reduction surgery be performed?
Since breast reduction surgery will require general anesthesia, it must be performed in an operating room that is part of a hospital institution or outpatient surgery center. Less frequently, patients may be operated on in an in-house office based operating room, but it is of utmost importance for patients to make sure that the office facility is accredited by a surgical accreditation body such as AAAASF.
What type of anesthesia will be used for my breast reduction surgery?
Routine breast reduction surgery requires the administration of a general anesthetic that will keep you asleep throughout the procedure.
What should I expect after breast reduction surgery?
After surgery, you will be taken into a recovery area where you will be closely monitored. Awaking from surgery, you may find small drainage tubes that are placed in your breasts in order to avoid the accumulation of fluids. Gauze dressings will be placed on your breasts and covered with an elastic bandage or surgical bra that must be worn for about 1 week after surgery. You may also experience a loss of sensation in your breast and nipple area, which is usually temporary. The incisions and tissue movement involved in the surgery may cause your breasts be become sore, swollen and bruised. Pain will be treated with medication prescribed by your plastic surgeon. Strenuous activity such as straining, bending and heavy lifting is off-limits for 3 to 4 weeks. Your stitches will be placed internally and externally you will find your incisions sealed with a sealant. Your incisions will remain red or pink for a few months after surgery. Your breasts will also require some time to assume a more natural shape.
When will I be able to return to work following breast reduction surgery?
Patients will have full recovery within 4 to 6 weeks of surgery. Patients will be able to return to work if it is not strenuous within two week of surgery. Patients will be allowed to wear a sports bra as early as 2 weeks following surgery and all routine undergarment following 4 weeks of surgery.
Are there any side effects associated with breast reduction surgery?
a) Numbness: Swelling after surgery usually results in loss of feeling in the breast and nipple area during the first several weeks. This impairment should be temporary and last no longer than a few months. In some cases, the loss of feeling can last longer or become permanent due to nerve damage as some sensory nerves are too small to be detected by the naked eye during surgery.
b) Scarring: Incisions may be lumpy and red for a few months, but they become less apparent over time and will usually fade to thin white lines. Healing scars can usually be covered completely by a bra or swim suit top. Please note that smoking impedes the healing process and typically results in more prominent and prolonged surgical scars.
c) Breast/Nipple asymmetry: Breasts may not be the same size and shape and nipples could be positioned unevenly depending on the degree of preoperative asymmetry. In general, symmetry is dramatically improved following breast reduction surgery.
d) Nursing problems: Women may not be able to breast-feed since the surgery removes a portion of the breast glands and milk ducts leading to the nipples.
Are there any risks associated with breast reduction surgery?
a) Hematoma: Hematoma refers to the accumulation of blood in the early postoperative period which pools into a pocket. Hematomas provide a perfect medium for harboring growth of bacteria. So if you have an infection anywhere in your body, the bacteria will travel through the blood stream and grow in the hematoma; this can lead to an infection as well as an open wound. In order to avoid a hematoma, drains can be placed in surgery so that any fluid accumulation can be drained. Drains are usually kept in place for 4 to 5 days. In addition, patients are checked preoperatively to make sure that they do not have a blood clotting deficiency. If blood clotting deficiencies are detected, then these can be corrected.
b) Seroma: Seroma formation refers to the accumulation of plasma fluid in pockets created by surgical elevation of the soft tissue and disruption of lymphatic vessels. This fluid accumulates due to a low blood count and protein deficiency, both of which may be present in breast reduction patients. This fluid can be a nuisance to patients requiring several aspirations in the office prior to their resolution. More importantly, these plasma fluid pockets may harbor bacterial growth and result in a clinical infection. Drains can be placed in surgery are very effective in preventing seroma formation.
c) Infection: An infection rarely occurs after breast reduction surgery. An infection may result in disruption of surgical incision lines and may leave the patient with an open breast wound especially at the middle and inferior aspect of the breast mound over the infra mammary crease line. Prolonged antibiotics and possible removal of antibiotics may be required to fight an infection and to prevent further extension of the infection. Risk of infections are avoided by using sterile technique, using intra-operative antibiotics, and sealing all incisions sites so that bacteria can’t get in through external contact. In addition, infections are less likely in patients who don’t smoke cigarettes or in smokers who quit smoking for at least 1 month prior to surgery.
d) Pulmonary embolism: Blood clots may form in leg veins during any surgery when the patient is under general anesthesia. Patients with a leg vein clot will complain postoperatively of pain in their calves. Patient’s with this complaint should be taken seriously and treated if a vein clot is diagnosed. Early treatment of patients with a deep leg vein will avoid migration of leg vein clot to the heart and lungs causing pulmonary embolism. Even though pulmonary emboli are rare, pulmonary emboli are the leading cause of death after surgery. Pulmonary emboli must be detected early by performing a CT Scan and should be treated urgently.
PATIENT-SPECIFIC QUESTIONS
What is breast reduction surgery?
Breast reduction surgery, or mammaplasty, is performed to reduce the size of large breasts and enhance their shape, symmetry, and proportionality to the rest of the body.
Will my insurance cover the cost of breast reduction?
Insurance companies usually cover the cost of a breast reduction when the purpose of breast reduction is to alleviate physical discomfort and pain caused by oversized breasts. A unilateral breast reduction should also be covered if the asymmetry resulted from a breast cancer operation. However, each medical insurance company has its own coverage criteria you will need to contact a Board Certified Plastic Surgeon, who will evaluate your needs and contact your insurance company to pre-determine coverage. Healthcare financing may also be available for breast reduction surgery motivated by medical need if your insurance covers only part, or none of your surgical cost. Unfortunately, recent changes in insurance policy have led to stricter criteria for breast reductive surgery candidates.
What is the youngest age that breast reductions are usually performed?
While breast reduction surgery is recommended to patients who have completed their breast development, the surgery can rarely be performed on a teenager who demonstrates grossly enlarged breasts, termed juvenile breast hypertrophy. In such cases, breast reduction surgery can be performed on patients as young as 14 or 15, depending on the severity of the symptoms and the maturity and determination of the patient. The typical patient presents after childbirth and completion of nursing and complains of enlargement of her breasts during pregnancy that did not return to their pre-pregnancy state.
What type of scarring should I expect?
The type of scarring depends on the type of breast reduction procedure performed. Traditional breast reduction surgery produces anchor-like scars that extend around the nipple, down the middle of the breast, and under the fold of the breast, termed the infra-mammary crease. Vertical incision breast reductions create shorter scars that also surround the nipple and extend vertically down the breast, but do not continue under the breast. Liposuction breast reduction usually leaves minor scars under the breast fold. Although scarring is a factor that should be considered by patients desiring breast reduction surgery, patients should keep in mind that surgical incisions are required to resect unwanted breast tissue. Additionally, scars that result from breast reduction surgery can usually be hidden under bras or bathing suit tops. Finally, sutures that are used today are far superior to those used less than a decade ago and allow plastic surgeons to achieve significantly lighter and thinner scars.
How is the nipple/areola sensitivity affected during breast reduction surgery?
In most cases, the nipple and areola remain attached to their nerves during the operation and thus are generally not affected by breast reduction surgery. The nipple and areola are usually moved by relocating the entire gland and supporting structures to a higher more aesthetically pleasing location on the breast mound. Loss of feeling in the nipple area usually persists for the first several weeks after surgery and no longer than a few months. In some cases however, permanent loss of nipple sensation may be caused by nerve damage as these nerves are extremely thin and not detectable by the naked eye.
Where are the incisions made during a breast reduction?
Traditional breast reduction surgery requires an incision that circles the areola, extends vertically downward toward the bottom of the breast, and continues under the fold of the breast, called the inframammary crease. This incision is anchor shaped and called an inverted-T incision. A second favorite technique termed the Vertical Reduction limits the incisions to around the areola and a single downward incision toward the bottom of the breast. Although this technique does limit the surgical incisions, it is limited to patients who have preoperative breast shapes that are wide in shape and not long in shape.
Are there any alternatives to the inverted-T incision?
The alternative to an inverted-T incision is a more novel technique called the Vertical Reduction. This method reduces the scarring significant by minimizing or even eliminating the incision beneath the breast when compared to the inverted-T incision.
How painful is breast reduction surgery?
Breast reduction surgery is typically performed on patients under general anesthesia. Postoperative pain following surgery is minimal as tissue dissection is limited to only the skin and fat and does not involve the muscle which is much more sensitive. Patients usually need limited pain medication after surgery and can return to work after about 2 weeks if their job does not require strenuous activity.
Do breast reductions require blood transfusions?
The need for blood transfusions during breast reduction surgery is extremely rare.
Does the breast reduction procedure require any medical tests prior to surgery?
On your initial visit, your surgeon will evaluate your health status by obtaining blood work. If you are 40 years or older or if you have had a personal or family history of breast symptoms (tenderness, lumps, nipple discharge) you will have to obtain a mammogram. Additionally, routine lab work such as EKG will be required if you are older than 55 years of age.
Is breast reduction by liposuction a good idea?
Liposuction breast reduction is a new procedure that has advantages of less scarring, increased likelihood of maintaining nursing ability, and a lower risk of losing breast and nipple sensation. However, liposuction only removes fat from the breast and is suitable only for patients that require mild breast reduction, have minimal skin looseness, and do not demonstrate drooping of the nipple and areola complex. Liposuction is more effective for younger women have may have enlarged breast tissue but maintain a tight breast skin envelope. Patients who need significant breast reduction will gain more substantial results with the traditional breast reduction method where both skin and underlying fat must be removed.