If you are a post-bariatric patient or an individual who requires a body lift, you may be wondering, “Will insurance cover a body lift?” This question warrants an understanding of a body lift as well as your insurance coverage. A body lift is done when a patient has excess, redundant, overhanging skin that is causing a functional problem.
This can be seen from weight loss patients or elder patients that do not have tight skin elasticity. Although heavy, redundant skin left behind after extreme weight loss may be aesthetically unpleasing, this is not enough justification for insurance coverage for body lifts. Insurance coverage for a body lift is only considered a medical condition if it causes discomfort due to recurrent rashes or if the redundant skin gets in the way of daily activities such as the use of your arms or walking, running, and exercise.
When the redundancy of the lower belly gets to be prominent, it is called a pannus. If the pannus covers your genitals such that it creates difficulty with sanitation, then this is considered a functional problem.
Now you may be wondering how do I find out whether my insurance will cover a body lift. This is because a majority of insurance providers do not cover a body lift operation. In general, if your insurance covers your bariatric surgery, then they should cover any skin related functional difficulties that arise from your weight loss. However, some insurance plans may exclude body lift procedures entirely.
As most plastic surgery procedures are considered elective and cosmetic, most body lifts procedures and tucks are not covered by insurance. With that being said, a body lift surgery after weight loss or post-bariatric surgery might be covered. A body lift surgery may involve Brachioplasty, breast lift, upper body lift, lower body lift, panniculectomy, and/or medial thigh tuck. These procedures may be considered medically necessary if you are having a functional deficit.
Newport Beach, board-certified plastic surgeon, Mirzania shares that at Cosmetic Plastic Surgery Institute, his private practice, he routinely observes that panniculectomies are covered by insurance. A panniculectomy is a surgery to remove the pannus, which is the described overhanging, excess skin, and tissue on the lower abdomen. These pants are sometimes referred to as an apron, as it overhangs below the belly and covers the genitals.
A panniculectomy does not tighten the muscles of the abdomen, which is a cosmetic procedure and also known as a tummy tuck with muscle plication, so it applies to a noncosmetic surgery. A medial thigh tuck may be covered if your skin and soft tissue fullness is creating difficulty with walking.
A Brachioplasty may be covered if you are having difficulty with the use of your arms. Breast lifts and lower body lifts are more difficult to get covered as they do not typically cause functional difficulties. Will insurance cover a body lift? You can only find out by seeing your plastic surgeon and submitting a coverage request.
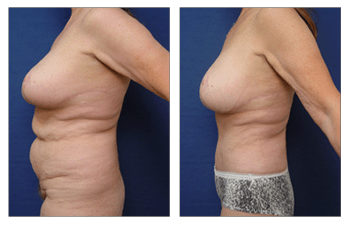
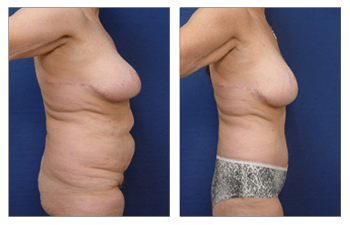
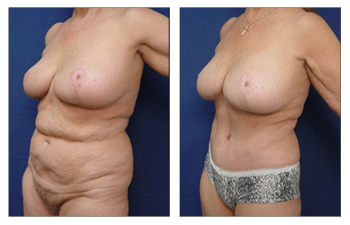
Please see this 65-year-old female status post-post-bariatric surgery with abdominoplasty with muscle plication and a breast augmentation revision.