WANT THE CONFIDENCE THAT COMES WITH
KNOWING YOU LOOK YOUR BEST?
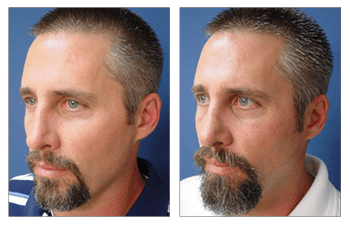
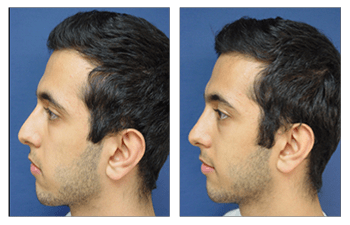
Crooked Nose CASE STUDIES
Crooked Nose
As a rhinoplasty surgeon, I have learned to become a keen listener. Although my patients have not had formal training evaluating nasal aesthetics, I am surprised at how accurately and intuitively they are able to identify nasal contour defects and to convey the changes that they desire. When I assess what I refer to as a suboptimal nasal contour, I am most focused on my patient’s dislikes and desired corrections.
Before I start my evaluation of your nose, I will typically ask you, "So what do you not like about your nose?" Infrequently, there may be some discrepancy between what you and I perceive as the ideal nasal shape. Providing knowledge of nasal aesthetics usually resolves any of these discrepancies.
In most situations, patients will find set standards for nasal aesthetics in agreement with their perceived aesthetics.
When you are thinking about what you don’t like about your nose, the most important decision that you need to make is whether you like the shape of your tip. If you desire removal of a nasal hump, narrowing of your nasal dorsum bridge/base, or correction of a crooked nose, then a closed rhinoplasty will suffice.
If you don’t like the shape of your nasal tip, then you should undergo an open rhinoplasty which can correct not only the nasal tip but also all of the former concerns. Many patients ask me why I don’t perform the open rhinoplasty procedure on all patients. This is an excellent question. Although the open rhinoplasty allows for correction of all nasal structures including the nasal tip, it does require more extensive dissection and trauma to the nose, several extra maneuvers, and longer operative times, which can be avoided if the nasal tip does not require alteration.
Conversely, for patients who do not require improvement in nasal shape, the closed rhinoplasty provides a less invasive and more affordable alternative solution to your nasal surgery needs.
Procedure
Improvement of nasal contour by various maneuvers including removing the nasal hump, narrowing the nasal base, and/or improving highlights of the nasal tip.
Length
Ranges between 1-2 hours (closed rhinoplasty) and up to 3 to 4 hours (open rhinoplasty) of operative time.
Anesthesia
General anesthesia is usually recommended as the breaking of the nasal bones is required to eliminate a nasal hump and reduce the nasal base width.
Place of Treatment
Outpatient surgical suite or hospital operating room.
Side Effects
1) Prolonged swelling up to 3 months is not uncommon due to poor lymphatic drainage especially following open rhinoplasty. Lymphatic drainage is compounded by extended surgical incision (open rhinoplasty) across the bottom of the nose (columella) when the nasal tip must be altered.
2) Temporary bruising is often associated with nasal surgery when nasal hump reduction and thus breaking of the nasal bones are required. Bruising is minimized by compression maneuvers during the operation, placement of an external splint following surgery, and icing of the eyes. Arnica gel is also recommended in patients who bruise easily. Most bruising subsides within 1 to 2 weeks.
Risks
1) Deep vein thrombosis (DVT) may occur in the legs immediately following surgery. DVT refers to the clotting off of leg veins which may result in compromised blood flow return from the legs; a more critical consequence may develop from this clot if it is dislodged and travels to the lungs causing a pulmonary embolus. Although rare, pulmonary emboli are the leading cause of death following surgery. Measures are taken intraoperatively to avoid such a complication.
2) Poor nasal scarring is seldom observed when the surgical incisions are extended to the bottom of the nose in order to refine the nasal tip shape (open rhinoplasty). Patients prone to scarring and thus individual genetics of healing are largely to blame for poor scarring.
3) Local skin infection is uncommon and associated with complex nasal deformities and thus more extensive nasal surgeries requiring augmentation of nasal parts with cartilage grafts. Diabetes and nutritional deficiencies are largely to blame for the difficult healing of these patients. When cartilage grafts are required, measures are taken intraoperatively to avoid this complication.
4) Residual nasal distortion is uncommon but associated with a preoperative crooked nose deformity. Despite measures taken to correct the crooked or twisted nose, the underlying cartilages which make up 2/3rd of the nasal infrastructure have “memory” and will try to mold back into their old shape. Several measures are taken to avoid this complication and include scarring (weakening) of the cartilage and “stitching down” the cartilage in its new desired shape.
Recovery
The recovery period for nasal surgery with a return to daily activities is usually 1 week. Patients are asked to forego physical activities and exercise for approximately 4 weeks until the nasal bones have completely fused and are stable.
Duration of Results
Patients who have undergone nasal surgery can expect aesthetically pleasing results for life. Early revisions are rare and are typically discouraged. Late revisions are only needed in younger patients whose noses continue to grow and evolve through life.
FREQUENTLY ASKED QUESTIONS
What is the history of nasal surgery (rhinoplasty)?
The first reported nasal surgery was performed by a physician named Sushruta who lived in ancient India around 500 B.C. Sushruta, who is often regarded as the «father of plastic surgery» began performing nasal surgery to reconstruct noses that had been amputated, an ancient punishment for criminals.
Am I a good candidate for nasal surgery (rhinoplasty)?
Most patients who seek nasal surgery (rhinoplasty) have a dislike of their external nasal contour. Some patients additionally have difficulty breathing. As such, patients who desire nasal surgery must have a thorough evaluation of not only their external nasal contour but also of their internal more functional structures.
Patient's nasal contour deformities and/or breathing difficulties may be developmental or arise from external trauma. Patients with external contour deformities may demonstrate an elongated nose, a short nose, a dorsal hump, a widened nasal base, up-turned nasal tip, down-turned nasal tip, crooked nose, twisted nose, and poorly defined nasal tip. Patients may also have concurrent breathing difficulty which will require concurrent surgical treatment during external nasal contouring.
What does nasal surgery (rhinoplasty) involve?
Nasal surgery (rhinoplasty) involves accessing and modifying the underlying infrastructure of the nose in order to improve external contour appearance. The nose is comprised of three segments which include the upper 1/3rd segments (bony infrastructure) versus the lower 2/3rd segments (cartilaginous infrastructure).
When the upper 2/3rd of the nose requires modification, then a «closed rhinoplasty» can be performed which uses incisions that are isolated to the inside of the nose. This incision bypasses the nasal tip infrastructure which cannot be modified by this technique.
When the nasal tip requires modification, then an open rhinoplasty is required which extends the internal incisions across the bottom of the nose (the columella), thus allowing the surgeon to completely peel up the nasal skin in order to directly visualize all of the infrastructural elements. Regardless of the technique chosen, the surgeon is able to modify exposed bony and cartilaginous structural supporting elements and thus alter the nasal contour appearance.
How do I plan for nasal surgery (rhinoplasty)?
On your initial visit, your surgeon will evaluate your health status by obtaining blood work. If you are 45 years or older your surgeon may order an EKG to rule out any heart conditions.
If you have had a history of breathing problems, your surgeon may order a CT scan to evaluate the status of your internal supporting structural elements specifically evaluating the septum (the central pillar). If you are a smoker, you should quit for 1 month prior to your nasal surgery to minimize the risks of infection especially if your surgery will require the use of cartilage grafts to reinforce your supporting structures.
In addition, it is prudent to quit smoking for 6 weeks following surgery to ensure a well-healed surgical incision. Finally, you will need to arrange for a friend if you don't have a spouse to care for any small children who may need to be lifted or carried as any possible risk of external trauma to your nose should be avoided.
How do I prepare for nasal surgery (rhinoplasty)?
Since your surgery will require general anesthesia, you must take several precautions prior to surgery. First, you will have to avoid eating and drinking after midnight on the day before surgery. This precaution ensures that your stomach is clear of digested foods that could potentially be aspirated and contaminate your lungs during the induction of anesthesia.
Since you will have anesthetic medications administered throughout the case, you will remain groggy for several hours and will require a ride to and from the surgery center. You should choose a caretaker who is conscientious and who can spend the first night with you.
What results can I expect after nasal surgery (rhinoplasty)?
Patients who undergo nasal surgery (rhinoplasty) are extremely satisfied with their surgery and their more proportioned nose and facial features.
By providing a thorough preoperative workup, safe intraoperative course, and frequent postoperative visits, patients should expect a speedy recovery and return to a more aesthetically proportional nasal contour and pleasing face. Patients are extremely pleased following nasal surgery(rhinoplasty) and demonstrate increased physical and mental confidence.
What type of anesthesia will be used for my nasal surgery (rhinoplasty)?
For the routine nasal surgery (rhinoplasty), the breaking (infracture) of the nasal bones requires general anesthesia. For certain individuals, desiring only nasal tip refinement a conscious sedation (sedation through intravenous medications only) will suffice.
Where will my nasal surgery (rhinoplasty) be performed?
Since nasal surgery (rhinoplasty) will require general anesthesia, it must be performed in an operating room that is part of a hospital institution or outpatient surgery center. Less frequently, patients may be operated on in an in-house office-based operating room, but it is of utmost importance for patients to make sure that the office facility is accredited by a surgical accreditation body such as AAAASF.
What should I expect after nasal surgery?
Patients will awaken from general anesthesia to find their nose covered by an external splint and a gauze dressing covering the nasal opening. The external splint acts like a cast and allows the nasal bones to set and heal much like a cast that you would get if you broke your arm.
The external splint also acts as a compression garment to eliminate any voids that could fill with blood and thus avoiding hematomas. The external splint is kept in place around the clock for the first 7 days.
Following your postoperative visit at 1 week following surgery, your splint will be removed and then is to be worn for another week only at nights. Swelling and bruising is typically minimal and resolves over the first week following surgery. Arnica gel is recommended for patients demonstrating increased bleeding interop in order to avoid excessive postoperative bruising. Patients are asked to avoid lifting weights greater than 15 pounds for the first two weeks. Additionally, patients are asked to avoid contact sports for the first 4 weeks in order to avoid compression of the nasal bones while they are setting and fusing.
For closed rhinoplasty, only absorbable sutures are used and do not require removal. For open rhinoplasty sutures used over the bottom of the nose (the columella) are removed at one week following surgery. Patients feel comfortable attending social engagements as early as two weeks following surgery. Although swelling is minimal following surgery, nasal tip swelling following open rhinoplasty will gradually resolve over the first three months.
When will I be able to return to work following nasal surgery (rhinoplasty)?
Patients can expect to return to work at 1 week following surgery once the external splint is removed and if they have a desk job. In general, patients are recommended to take 10 days off if their work permits. Weight restriction of 15 pounds for the first two weeks is recommended for patients who may have more physical jobs.
Are there any side effects associated with nasal surgery (rhinoplasty)?
There are several side effects that have been associated with nasal surgery (rhinoplasty) and included:
a) Prolonged swelling up to 3 months is not uncommon due to poor lymphatic drainage especially following open rhinoplasty. Lymphatic drainage is compounded by extended surgical incisions used in open rhinoplasty and placed across the bottom of the nose (columella) when the nasal tip must be altered.
b) Temporary bruising is often associated with nasal surgery when nasal hump reduction and thus breaking of the nasal bones is required. Bruising is minimized by compression maneuvers during the operation, placement of an external splint following surgery, and icing of the eyes. Arnica gel is also recommended in patients who bruise easily. Most bruising subsides within 1 to 2 weeks.
c) Numbness: Numbness of the nasal dorsum and tip occur when sensory nerves are transected by virtue of elevating the nasal skin off of the underlying structural support elements. Since these nerves are microscopic in size, they cannot be visualized during nasal dissection. Fortunately, numbness is temporary and resolves itself over 2 to 3 months as the nerve endings grow back into the nasal skin.
d) Surgical scar redness: Hyperemia of the incision over the bottom of the nose (the columella) is to be expected and will resolve over the first month. Layered closure of the incision line is performed in order to minimize the tension of the incision line and to enhance incision healing. Avoiding cigarette smoking for one month prior to surgery and six months following surgery is essential to optimizing healing.
Are there any risks associated with nasal surgery (rhinoplasty)?
a) Postoperative bleeding may occur following nasal surgery since the nose has numerous blood vessels supplying it. Appropriate clotting of these vessels (hemostasis) during the operation avoids postoperative bleeding. In addition, external compression provided by the external nasal splint further prevents postoperative bleeding. Finally, patients are tested preoperatively to ensure that they do not have a bleeding disorder. For patients identified as having a bleeding tendency, intraoperative administration of DDAVP (a blood clotting factor) is administered to avoid bleeding complications.
b) Deep vein thrombosis (DVT) may occur in the legs immediately following surgery. DVT refers to the clotting off of leg veins which may result in compromised blood flow return from the legs; a more critical consequence may develop from this clot if it is dislodged and travels to the lungs causing pulmonary emboli. Although rare, pulmonary emboli are the leading cause of death following surgery. Measures are taken intraoperatively to avoid such a complication.
c) Poor nasal scarring is seldom observed when the surgical incisions are extended to the bottom of the nose in order to refine the nasal tip shape (open rhinoplasty). Patients prone to scarring and thus individual genetics of healing are largely to blame for poor scarring.
d) Local skin infection is uncommon and associated with complex nasal deformities and thus more extensive nasal surgeries requiring augmentation of nasal parts with cartilage grafts. Diabetes and nutritional deficiencies are largely to blame for the difficult healing of these patients. When cartilage grafts are required, measures are taken intraoperatively to avoid this complication.
e) Residual nasal distortion is uncommon but associated with a preoperative crooked nose deformity. Despite measures taken to correct the crooked or twisted nose, the underlying cartilages which make up 2/3rd of the nasal infrastructure have memory and will try to mold back into their old shape. Several measures are taken to avoid this complication and include scoring (weakening) of the cartilage and «stitching down» the cartilage in its new desired shape.
PATIENT-SPECIFIC QUESTIONS
How does rhinoplasty effect breathing?
Nasal surgery involves alteration of the underlying infrastructure which not only affects the external contour aesthetics but also the internal airway functionality.
The internal infrastructure directly affects the internal airway opening diameter and thus airflow. The internal nares can be thought of as two tubes that allow air to flow in and out. When these tubes are well supported and smooth, then the airflows in without turbulence. However, when the nose is crooked, twisted, collapsed, overly long, then airflow is compromised by turbulence. Air turbulence further irritates the nasal lining(mucosa) further inflaming the walls and decreasing the tube diameter.
As a result, even when patients seek the only improvement of the external nasal contour, they often remark on the improvement of their breathing.
Does nasal surgery (rhinoplasty) last forever?
Nasal surgery performed to correct the external contour aesthetics involves correction of the underlying infrastructure The underlying structures are compromised of nasal bones over the upper 1/3rd and cartilaginous structures over the lower 2/3rd.
Whereas alteration of the nasal bones which are rigid is stable, alteration of cartilage components is considered more malleable. Cartilaginous structures are not only pliable and less rigid but they also maintain «memory» of their prior shape.
As a result, when changes in cartilaginous structures are performed, several steps are taken to reinforce these structural changes. Changes in cartilage shape are secured by utilizing techniques to weaken unwanted shapes (by scoring the cartilage) and by reinforcing new desired shapes (with suture fixation).
Regardless, when a crooked nose is fixed and aligned, there is a risk that the aligned nose may minimally deviate to its prior shape. In addition, long term changes in the nose are possible over decades as the nose is one of the body organs that continues to grow with age.
Does nasal surgery require internal splints?
Although internal splints were a mainstay of nasal surgery in the past, today, internal splints are no longer routinely utilized. In contrast, external splints are routinely utilized to maintain the contour changes completed during surgery until the nasal bones set and fuse in their new position.
Internal splints have been associated with a more difficult postoperative recovery by inhibiting breathing ability and also associated with external distraction (lateralization) of the nasal bones negating attempts to narrow the nasal base.
Internal splints are only used to ensure straight alignment of the nose following correction of a complicated crooked or twisted nose as these noses have a tendency to return to their preoperative shape due to cartilage memory.
How can the results of nasal surgery (rhinoplasty) be assessed?
Standardized photographs are typically obtained to assess the effects of nasal surgery (rhinoplasty). Typical views include an AP (anteroposterior- straight-ahead view), 2 lateral profile views, 2 oblique profile views, birds-eye view (taken from the bottom up), and worm's eye view (taken from the top-bottom). Nasal contour improvements can be assessed by viewing the pre and postoperative sets of these views.
What is the desired look for the nasal tip?
Nasal tip shape alterations are indicated to provide «highlights» to the nasal tip, which involves decreasing tip fullness and/or improving ill-defined tip features associated with obtuse shaped underlying cartilages.
Tip defining points represent shine spots at the most projected aspect of the tip which is created by the shadowing/ effects created by outside lighting. Tip defining points are considered aesthetically pleasing when spanning a distance of 4 to 6 mm depending on the overall size of the nose and gender of the patient.
Can nasal surgery worsen breathing ability?
Functional breathing compromise can develop if the patient develops a pinched nose deformity. This complication follows the excessive reduction of the tip and bottom 1/3rd cartilages.
Another cause of breathing compromise is caused by the collapse of the middle 1/3rd cartilage structural elements. Preoperative analysis of this region can warn the surgeon against this complication.
The propensity for this complication can be detected by performing the Cottle test maneuver, which results in improved breathing capacity when the medial cheeks are pulled outward.
What happened to Michael Jacksons nose?
Whenever surgery is performed on the skin and underlying tissues such as in the nose, the tissues become slightly thinner in thickness. This thinning effect gets compounded when multiple surgeries are performed in the same area.
The skin thins out, and pretty soon, you literally see the underlying cartilage sticking out. That's what went wrong with Michael. The lesson learned that you want to get it right the first time.
Why are revision rhinoplasties so common?
The nose is very complex in its structure and dynamics so that the nose can change over time if not adequately supported. The supporting structural elements must be reinforced during rhinoplasty especially during open rhinoplasty.
Surgeons who were trained only to perform closed rhinoplasties and who are now performing open rhinoplasties tend to make this mistake.
Why do some rhinoplasties cause the nose to look like a pig nose?
The relationship of the nose to the upper lip is critical. The angle created by the upper lip to the nose(the nasolabial angle) has been studied and should be set at 95 degrees in men and 105 degrees in women.
When this angle is judged inappropriately and set at greater than 105 degrees (more obtuse) then the pig nose results.
Who do some women end up with sky slope noses?
The top of the nose (nasal dorsum) should be set at 1 to 2 mm below the tip of the nose. In men, the top of the nose should be straight but in women, there may be a slight slope (concavity).
However, inexperienced surgeons may inappropriately exaggerate this slope thus giving their patients an undesired sky slope look.
Is there a minimum age when nasal surgery (rhinoplasty) can be performed?
Rhinoplasty should not be considered for patients until they become adults (age 18 and older). This is because patients have to demonstrate the maturity required by changing the appearance of such a vital facial structure located at the center of their face. The perception of beauty and the capacity to cope with ensuing results is not a trivial matter!
Why do some postoperative noses droop following nasal surgery?
The problem of the droopy postoperative nose is unfortunately all too common. The nasal tip is relatively heavy when compared to the other parts of the nose.
Thus, when changing the structural elements in an attempt to alter the shape of the nose, the surgeon must be careful to not compromise the structural stability of the nose. This concept is most important following open rhinoplasty surgery where several measures must be taken to reinforce the nasal tip structural elements.
Surgeons trained in only closed rhinoplasty and who are not accustomed to open rhinoplasty principles are most likely to achieve this complication.