WANT THE CONFIDENCE THAT COMES WITH
KNOWING YOU LOOK YOUR BEST?
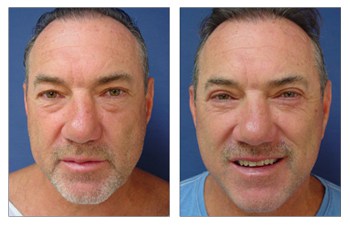
Lower Eyelid CASE STUDIES
Lower Eyelid
Lower blepharoplasty is intended for patients who have observed wrinkly and/or puffy lower eyelids. Much like the face and upper eyelid, the aging lower eyelid is plagued by an accumulation of redundant skin and loosened underlying eyelid muscles, resulting in herniation of fat pockets; this herniation can result in unsightly puffiness of the lower eyelids called festoons.
Patients are typically recommended to undergo a combination of removal of skin and conservative resection of redundant fat pockets. Finally, a deep groove can be observed along the medial edge of the eyelid that extends onto the mid-cheek, called the nasojugal groove; this groove can be filled using the above removed and unwanted fat.
Lower blepharoplasty is an intricate surgery, as the lower eyelids are vulnerable to undesirable side effects. The surgeon has to operate a fine line when removing redundant eyelid skin so that enough skin is removed to create a rejuvenated eyelid contour, without causing an ectropion, a lower eyelid deformity resulting from the excessive pull and downward drag of the lid margin. This deformity can be quite disfiguring to a patient. As such, Dr. Paris utilizes an oblique vector of pull on the redundant skin, which allows for the tension on the resultant eyelid skin to be transferred from a vertical (more susceptible to ectropion) to a more horizontal plane. This maneuver allows Dr. Paris to remove appropriate redundant skin while minimizing the risk of ectropion.
In addition, during your consultation, Dr. Paris will determine if you have any risk factors for developing ectropion. These include a loose lid margin which is evaluated by performing a lower eyelid “snap back” test.
Another risk factor includes poor cheekbone support which is the foundation of your eye globe. When the cheeks bones are weak, then the lower eyelids are more vulnerable to ectropion.
For patients that demonstrate risk factors for ectropion, Dr. Paris will advocate a lid tightening procedure, called a canthopexy, to be performed simultaneously during your lower blepharoplasty. In summary, a comprehensive analysis of the lower eyelid is required during your consultation to accurately convey an effective and safe improvement in your lower eyelid appearance.
| Procedure: | Improvement in lower eyelid contour with resolution of eyelid bulges, upper eyelid hollow, and redundant skin by strategic resection of redundant skin, resection and/or repositioning of droopy eyelid fat, and suspension of eyelid muscle. |
| Length: | Ranges between 1 to 2 hours. |
| Anesthesia: | General anesthesia. |
| Place of Treatment: | Outpatient surgical suite or hospital operating room. |
| Side Effects: | 1) Inability to close the eye is usually temporary and subsides over 1 to 2 weeks.
2) Redness of the incision lines may be noticeable extending beyond the lash line and may persist over the 1st month following surgery. 3) Residual asymmetry of the lower eyelids may be present if asymmetry was pronounced preoperatively. |
| Risks: | 1) Deep vein thrombosis (DVT) may occur in the legs immediately following surgery when general anesthesia is used. DVT refers to the clotting off of leg veins which may result in compromised blood flow return from the legs; a more critical consequence may develop from this clot if it is dislodged and travels to the lungs causing a pulmonary emboli. Fortunately, this risk is avoided by the use of pneumatic compression boots that minimize this complication.
2) Severe eyelid drooping: Severe lower lid drooping(ectropion) is a result of over aggressive resection of the redundant lower eyelid skin or damage to the motor nerves of the lower eyelid closing muscle (orbicularis oculi). When this complication is not helped by message and taping of the lower eyelid, then lower lid tightening, repositioning, and/or even lower lid skin grafting may be necessary to resolve this complication. 3) Bleeding or small hematoma may occur and refers to the accumulation of blood in the early postoperative period which pools into a pocket. Since the skin of the eyelid is limited, hematomas must be drained immediately as any increased build up of fluid may result in disruption of your incision line and/or increase pressure on the eye globe itself. 4) Infection: An infection can occur following lower eyelid surgery but is very rare. The eyelid tissue as is the facial skin is very well vascularized and not likely to get infected. In addition, lower eyelid patients are provided antibiotic eyedrops which should suppress any potential bacterial growth. 5) Dry eyes: Dry eyes may develop as a result of changing pressures on the eyeball caused by the tightening of the overlying eyelid skin. The increase in pressure is believed to affect the eye lubrication and draining system (lacrimal system) which keep the moistened at all times. Patients who have a propensity for dry eyes preoperatively should be cautioned about developing this complication. Fortunately, as the eye accommodates to its new state, dry eyes tend to resolve over several months. 6) Visual compromise: Although this an extremely rare complication, it is conceivable that direct damage to the globe of the eye and/or the vascularity of the globe could occur resulting in blindness. |
| Recovery: | The recovery period for lower eyelid surgery with a return to most daily activities is around 4 to 5 days. Patients will typically return to work within 10 days following surgery. |
| Duration of Results: | Patients who have undergone lower eyelid surgery can expect aesthetically pleasing results for life. Early revisions are rare and are typically discouraged. Patients will notice turning back of the clock of approximately 15 years following lower eyelid surgery and will notice a natural return of the aging process. |
FREQUENTLY ASKED QUESTIONS
Am I a good Candidate for lower eyelid surgery?
In order to determine if you are a good candidate, your lower eyelid consultation will require evaluation of several items. First, the surgeon must assess degree of skin redundancy or flaccidity. This will determine the extent of skin incision required to remove the redundant skin. This length of the incision is significant as it not only spans along the lash line where it is hidden, but also extends beyond the lash line over the lateral cheek where it is visible. In addition, the surgeon must assess the degree of fat herniation that is present over three separate fat compartments located in the lower eyelid. These herniated fat pads result in a bulge that is present in some patients seeking lower eyelid surgery and is termed, the festoons. Your surgeon may utilize a combination of conservative resection and redraping of this fat in order to reduce the bulge. Finally, the surgeon must assess the degree of hollow that may be present below the bulge, termed the nasojugal groove. This groove is created by the above bulge, and the fact the loss of cheek prominence as the facial skin and fat is pulled down the face by the effects of gravity and aging. When this groove is minimal to moderate, suspension of the muscle of the eye (orbicularis oculi) allows for the effacement of this groove. When severe, it may be necessary to combine lower eyelid surgery with an elevation of this fallen cheek pad using a faceliftor midface cheek lift. Good candidates for lower eyelid surgery should not have recent visual acuity changes and no difficulty with dry eyes. In addition, ideal patients for lower eyelid surgery should not have increased lower lid laxity or lid sagging, termed ectropion, which can be judged by your plastic surgeon by performing a series of maneuvers (lid snap back test). If lower eyelid laxity is present, then a lower lid tightening procedure may be necessary. Finally, the lie of the lateral aspect of the eyelid must be evaluated and if down turned, the lateral aspect of the eyelid(lateral canthus) may have to be repositioned, termed lateral canthoplasty/canthopexy. Patients must be aware that several risk factors may be present predisposing the patient to higher complication rates. Surgeons should identify these and discuss them with their patients preoperatively and include: a loose lower lid margin, a sagging lower eyelid margin, a down turned lateral eyelid corner, a large eyeball, and/or poor cheek bony support.
What does lower eyelid surgery involve?
The lower eyelid procedure incorporates removal of redundant skin, conservative resection or redraping of the fat, and possible suspension of the underlying muscle. In cases of lower eyelid margin laxity, a lower lid shortening procedure maybe performed. If the lateral corner of the eyelid is downturned, then the lateral eyelid, lateral canthus, may have to be repositioned. While waiting in the preoperative area, the patient is asked to sit up so that skin redundancy of the lower lid skin and degree and position of lower lid fat herniation can be marked. After induction of anesthesia, the lower eyelid incision is made over the lateral aspect of the eye lid and carried along the bottom of the lash line. The lower eyelid skin is then elevated in order to allow access to the underlying fat pads. Prior to trimming of the skin, three separate compartments of fat lying under the eye muscle, called the orbicularis oculi muscle, are assessed and herniated fat is either conservatively resected or redraped as necessary to eliminate the bulge. Next, the eye muscle is resuspended if necessary to eliminate the moderate eye hollow if it is present on preoperative analysis. Finally, the redundant skin of the lower eyelid is redraped and trimmed as necessary. It is important to avoid over-resection of the lower eyelid skin which will result in postoperative sagging of the lower lid margin, termed ectropion. Meticulous repair of the skin incision is required to allow for optimum results. Eyes that are demonstrate risk factors as discussed above, may require further surgical maneuvers to either shorten, tighten, or redirect the lower eyelid margin.
How do I plan my lower eyelid surgery?
On your initial visit, Dr. Paris will evaluate your health status, determine the amount of skin redundancy, fat herniation, and presence of lower eyelid surgery risk factors. In addition, the surgeon will check your blood work to make sure that you are not a surgical risk and that you do not have bleeding tendencies. If you are a smoker, then you should quit for 1 month prior to lower eyelid surgery in order to allow your body adequate time to rid itself of any residual nicotine. Nicotine in your system results in shutting off of small blood vessels which carry nutrients to the skin; this may result in longer healing times and prolonged redness of your eyelid incision line.
How do I prepare for lower eyelid surgery?
Since your surgery will require general anesthesia, you must take several precautions prior to surgery. First, you will have to avoid eating and drinking after midnight on the day before surgery. This precaution ensures that your stomach is clear of digested foods that could potentially be aspirated and contaminate your lungs during induction of anesthesia. Since, you will have anesthetic medications administered throughout the case, you will remain groggy for some time and will require a ride to and from the surgery center if you elect not to commit to an overnight stay on the premises. Finally, you may experience moderate degree of swelling for the first day following your surgery. You should choose a caretaker who is conscientious and who can spend the first night with you.
What results can I expect after lower eyelid surgery?
Following lower eyelid surgery, patients can expect a smooth and youthful lower eyelid contour. As your swelling resolves over the first 48 hours, you will be pleasantly surprised at the degree of youthfulness that your lower eyelid surgery will provide your entire mid and upper face.
Where will my lower eyelid surgery be performed?
Since your surgery will require general anesthesia, it must be performed in an operating room that is part of a hospital institution or outpatient surgery center. Less frequently, patients may be operated on in an in-house office based operating room, but it is of utmost importance for patients to make sure that the office facility has been accredited by a surgical accreditation body such as AAAASF.
What type of anesthesia will be used for my lower eyelid surgery?
Since your surgery involves removal of manipulation of not only skin but also orbital fat and muscle, you will require general anesthesia. In addition, the surgeon’s incision is extremely close to your field of vision (surgical incision placed just under the lash line), and thus makes it very difficult for the patient to tolerate if he/she is awake.
What should I expect after lower eyelid surgery?
When you wake up from anesthesia, expect to find it difficult to see as there will be lubricant ointment in your eyes to protect your eyes and to keep them moistened. In addition, patients should expect moderate degree of swelling that may partially close the eyes resulting in limited visual field. Swelling will be minimized by use of ice packs around the clock. In addition, antibiotic and lubricant eye drops are recommended to avoid postoperative infections and to avoid drying of the eyes. You may feel some tightness around the eyes as the skin around the eye globes has been tightened and the eye globe must acclimatize to its new environment. Expect your sutures to be removed within the first 7 to 10 days and return to normal activities within 10 days.
When will I be able to return to work following lower eyelid surgery?
Patients undergoing standard lower eyelid surgery should expect to return to work no earlier than 10 days following surgery. Unlike the upper eyelid surgery, the lower eyelid surgery is associated with significantly more bruising and swelling. As such, most patients find it necessary to remain out of work for longer period until most cheek swelling and bruising has resolved.
Are there any side effects associated with lower eyelid surgery?
There are several side effects that have been associated with lower eyelid surgery and these include:
a) Inability to close eyes (lagophthalmos) is usually a temporary condition that is common over the early period following surgery. Patients may note quick resolution of this difficulty when it is caused by paralyzed muscles that will recover once the local anesthetic wears out in a few hours. Minimal lagophthalmos may be present and will resolve over one week. Minimal degree of lagophthalmos may be created by pulling of the lower eyelid, termed ectropion. This degree of sagging of the lower eyelid may be secondary to postoperative swelling or created by aggressive reduction of the lower eyelid skin resulting in pulling down the lower eyelid margin. When ectropion is minimal, manual message and taping over the first two weeks will result in resolution of symptoms.
b) Redness of incision lines may persist while the incision line is healing over the first month following surgery. Although the incision lines just under the lash line (sub-cilliary incision) are nearly invisible, the extension of the incision line past the lash line which is necessary to removed redundant skin may remain red for approximately two weeks. Smokers who do not quit smoking for 4 weeks prior to and 6 weeks following surgery are prone to this annoyance.
c) Asymmetry of the eyelids may be present postoperatively only when there is asymmetry present preoperatively. In general, patients should expect near perfect symmetry as the surgeon will make all attempts to correct any residual asymmetry. As such, patients should realize that upper eyelids are not always identical and minimal asymmetry may be present.
Are there any risks associated with upper eyelid surgery?
a) Deep vein thrombosis (DVT) may occur in the legs immediately following surgery when general anesthesia is used. DVT refers to the clotting off of leg veins which may result in compromised blood flow return from the legs; a more critical consequence may develop from this clot if it is dislodged and travels to the lungs causing a pulmonary emboli. Fortunately, this risk is avoided by the use of pneumatic compression boots that minimize this complication.
b) Severe ectropion: Severe lower lid sagging(ectropion) is a result of over aggressive resection of the redundant lower eyelid skin or damage to the motor nerves of the lower eyelid closing muscle (orbicularis oculi). When this complication is not helped by message and taping of the lower eyelid, then lower lid tightening, repositioning, and/or even lower lid skin grafting may be necessary to resolve this complication.
c) Bleeding or small hematoma may occur and refers to the accumulation of blood in the early postoperative period which pools into a pocket. Since the skin of the eyelid is limited, hematomas must be drained immediately as any increased build up of fluid may result in disruption of your incision line and/or increase pressure on the eye globe itself.
d) Infection: An infection can occur following lower eyelid surgery but is very rare. The eyelid tissue as is the facial skin is very well vascularized and not likely to get infected. In addition, lower eyelid patients are provided antibiotic eyedrops which should suppress any potential bacterial growth.
e) Dry eyes: Dry eyes may develop as a result of changing pressures on the eyeball caused by the tightening of the overlying eyelid skin. The increase in pressure is believed to affect the eye lubrication and draining system (lacrimal system) which keep the moistened at all times. Patients who have a propensity for dry eyes preoperatively should be cautioned about developing this complication. Fortunately, as the eye accommodates to its new state, dry eyes tend to resolve over several months.
f) Visual compromise: Although this an extremely rare complication, it is conceivable that direct damage to the globe of the eye and/or the vascularity of the globe could occur resulting in blindness.
PATIENT SPECIFIC QUESTIONS
Can children get baggy upper eyelids?
There exists a rare inherited disorder in children, called Blepharochalasis, which results in baggy upper eyelids. Children develop repetitive episodes of eyelid swelling that eventually stretches out all the tissues of the eyelid including, the skin, muscle, and structurally supporting tendons. These children often need a more complex reconstructive upper eyelid surgery.
What does upper eyelid surgery involve?
The upper eyelid procedure incorporates eliminating excess skin and conservative removal of protruding eyelid fat. Amount of upper eyelid skin removed is dependent on the degree of skin laxity. While waiting in the preoperative area and while the client is awake, the amount of redundant skin can be marked so that over resection of skin is avoided. Recent studies on aging have revealed a propensity for loss of overall fat volume in the face and eyes. These studies have prompted surgeons to be more conservative with removal of protruding eyelid fat. Many older clients who had more aggressive removal of fat are now returning to surgeon’s offices with a hollowed out appearance of their upper eyelid, termed the “gaunt” look. Fat pads in the upper eyelid are found in the central(middle) and medial(next to the nose) compartment. Today, conservative removal of fat is advocated and usually involves the medial fat pad only.
How long do I have to take off of work for upper eyelid surgery?
The traditional upper eyelid involves removal of upper eyelid skin and minimal fat pad and is considered minimally invasive. Subsequently recovery is considered short and most patients are able to return to work within two to three days. Patients may elect to avoid important social engagements as small, clear sutures are removed at one week following surgery.
If I am planning facelift surgery can I be considered for an upper eyelid surgery?
Patients undergoing facelift surgery will realize a more youthful facial and neck contour. If the upper eyelids demonstrate signs of aging, then patients may find a discontinuity of their youthful face and neck following facelift surgery when compared to their aged upper eyelid contour. Patients are encouraged to consider upper eyelid surgery at the time of their facelift surgery if upper eyelid aging signs are present.
How does a forehead lift effect the upper eyelid contour?
Patients considering upper eyelid surgery should have a thorough evaluation of their brows. A lowered brow position will increase the degree of upper eyelid skin present. In contrast, surgery to lift the eyebrows, i.e. forehead lift, results in reducing the redundant upper eyelid skin. As a result, patients who undergo forehead and eyelid surgery synchronously, will have their eyebrows lifted prior to their upper eyelid surgery. This will then result in more conservative resection of the upper eyelid skin.
Will I have difficulty closing my eyes following upper eyelid surgery?
Temporary tightness of the upper eyelid skin is not uncommon. If patients experience tightness they will notice relaxation of their upper eyelid skins and complete closure within one week. In the early period, it may be prudent to place eye lubrication into the eyes in order to prevent scleral abrasions.
Where is my upper eyelid incision made?
Upper eyelid surgery requires excision of redundant upper eyelid skin. Excision lines are placed strategically so that the final surgical incision line will fall in the natural upper eyelid crease (termed the supratarsal crease). This allows for improvement of upper eyelid contour using a nearly invisible surgical incision line.
If I have thyroid disease can I still be considered for lower eyelid surgery?
Patients who have thyroid disease often present with enlarged eyeballs, medically termed proptosis. Patients with enlarged eyeballs have to be examined thoroughly preoperatively as they have an increased risk of developing an undesirable “pulled look” of their lower eyelid following lower eyelid surgery (termed ectropion). These patients may require a lower lid tacking procedure to supplement the routine lower eyelid surgery. Consultation with a board certified plastic surgeon is necessary to determined what maneuvers will be required intraoperatively to ensure an aesthetically optimum result.
If I am planning to have a facelift surgery can I be considered for a lower eyelid surgery?
If you are planning to undergo facelift surgery, you should be considered for having your lower eyelid surgery performed at the same time. Although facelift surgery utilizing the extended “high” SMAS facelift technique will result in removal of some lower eyelid hollow, often a lower eyelid surgery is also beneficial to remove redundant skin that may become even more apparent following facelift surgery.
Will I have any numbness following lower eyelid surgery?
Numbness of the lower eyelid skin following lower eyelid surgery is uncommon and usually temporary. Numbness immediately following surgery is secondary to postoperative swelling that is expected and which will resolve over the first several weeks.
Will my lower eyelid hollow be improved following lower eyelid surgery?
Patients who present desiring lower eyelid surgery often complain of redundant skin, bulging of the upper aspect of the lower eyelid skin, and hollow of the lower aspect of the lower eyelid skin.
What lower eyelid changes can I expect to change with lower eyelid surgery? Lower
Lower eyelid surgery will remove bagginess, fatty protrusions, upper face hollowness, lax hanging skin, and improve over all lower eyelid contour.
What is Blepharochalasis?
Blepharochalasis is a rare inherited disorder that appears in childhood; children will notice repetitive episodes of eyelid swelling that eventually leads to loosening of eyelid muscles that help lift the upper eyelid (levator muscle). Eventually, these children will notice drooping of their eyelids.
What is Dermatochalasis?
Dermatochalasis refers to the stretching and redundancy of eyelid skin associated with aging changes.
What is Steatoblepharon?
Steatoblepharon is the medical term for herniated eyelid fat that protrudes under the eyelid skin and results in puffiness of the lower eyelids.
What is eyelid ptosis?
Eyelid ptosis refers to the drooping of the upper eyelid margin that is caused by stretched out or weakened muscle of the eye which helps lift the eyelid (levator muscle). This condition must be detected by your plastic surgeon prior to surgery as it will require tightening of your muscles in addition to the removal of the redundant skin and protruding fat pad.
How many fat compartments exist in the eyelids?
There are two fat compartments in the upper eyelid and three in the lower lid. If performed by non-trained physicians, the lacrimal gland located over the lateral aspect of the outer aspect of the eyelid may be confused as a fat compartment. Inadvertent injury to the lacrimal gland will result in dry eye syndrome.
How can someone go blind during eyelid surgery?
Although this complication is rare and devastating, it is observed following bleeding into the orbital socket likely caused by bleeding from a blood vessel around the eyelid fat compartments. Bleeding in this compartment is termed retrobulbar hemorrhage and may lead to collapse of the vessels that feed the eye globe if sufficient pressure accumulates in this space. Risk factors include high blood pressure or poor blood clotting capacity. If caught early, then release of the eyelid incisions and possible release of the lateral aspect of the eyelid margin (cantholysis), and infusion of a diuretic are necessary to prevent permanent damage.
Are there different causes for upper eyelid droop (ptosis)?
Several causes for upper eyelid droop exist and have been characterized as:
1) Myogenic (dysmyogenic) ptosis: most common congenital type, due to faulty development of the eyelid muscle that pulls the eyelid up (levator muscle).
2) Neurogenic ptosis: results from faulty innervation of upper eyelid lid retractors; ptosis is profound with complete interruption of innervation to levator muscle.
3) Mechanical or traumatic ptosis: results from any traumatic injury that interferes with levator muscle or its innervation;
What is postsurgical lagophthalmos?
This refers to the inability to close eyelids completely or to cover the globe adequately. It is common postoperatively due to swelling of the eyelid following surgery. If it does not resolve over the first several weeks it can be caused by over-resection of the upper eyelid redundant skin. Patients are provided artificial tears and/or lubricating eye ointment for routine surgical aftercare while this condition resolves.
What creates the natural upper eyelid crease?
The natural upper eyelid crease is called the supratarsal fold or crease. This crease occurs just above the upper border of a stiff structure called the tarsus. The tarsus provides structural integrity to the lower aspect of the upper eyelid so that it has stiffness and so that it does not flop around. This crease is created by the extension of the eyelid lifting muscle, called the levator, as it attaches to the skin.
What is the double eyelid operation?
This operation is often requested by patients of Asian ancestry who lack a supratarsal fold, the naturally occurring crease of the upper eyelid. This occurs because the eye lifting muscle, the levator, has either lost its attachments to the skin or the attachments are lower on the eyelid over the tarsus, the stiff portion of the lower aspect of the upper eyelid, thus not allowing for the naturally occurring crease to occur, or do not have the fold bilaterally; When the fold then is present, this creates two aesthetically pleasing segments to the upper eyelid referred to as the double eyelid. which is considered aesthetically normal. The double eyelid operation uses standard upper eyelid surgery techniques with the addition of re-establishing the levator connection to the upper eyelid skin.